Our Research
Software Implementation and User Perception
The implementation of a haptic feedback virtual reality simulation clinic with dynamic patient interaction and communication for medical imaging students.
Sapkaroski, D., Baird, M., McInerney, J., & Dimmock, M. R. (2018). The implementation of a haptic feedback virtual reality simulation clinic with dynamic patient interaction and communication for medical imaging students. Journal of medical radiation sciences, 65(3), 218-225. doi:10.1002/jmrs.288
An immersive virtual reality (VR) simulation clinic with dynamic patient interaction and communication was developed to facilitate the training of medical radiation science students. The software “CETSOL VR Clinic” was integrated into the Medical Imaging programme at Monash University in 2016 in order to benchmark student experiences against existing simulation techniques (ShaderwareTM).
Methods: An iterative approach to development, based on two cycles of user feedback, was used to develop and refine the simulated clinical environment. This environment uses realistic 3D models, embedded clinical scenarios, dynamic communication, 3D hand gesture interaction, gaze and positional stereoscopic tracking and online user capabilities using the UnityTM game and physics engines. Students’ perceptions of educational enhancement of their positioning skills following the use of the simulation tools were analysed via a 5-point Likert scale questionnaire.
Results: Student perception scores indicated a significant difference between simulation modalities in favour of the immersive CETSOL VR Clinic, v2 (4,N = 92) = 9.5, P-value <0.001.
Conclusion: Student perception scores on improvement of their clinical and technical skills were higher for the hand positioning tasks performed with the CETSOL VR ClinicTM than with the comparative benchmark simulation that did not provide dynamic patient interaction and communication.
User Performance Outcomes
Quantification of Student Radiographic Patient Positioning Using an Immersive Virtual Reality Simulation. Simulation in Healthcare.
Sapkaroski, D., Baird, M., Mundy, M., & Dimmock, R., M. (2019). Quantification of Student Radiographic Patient Positioning Using an Immersive Virtual Reality Simulation. Simulation in Healthcare., 14(4). doi:10.1097/sih.0000000000000380
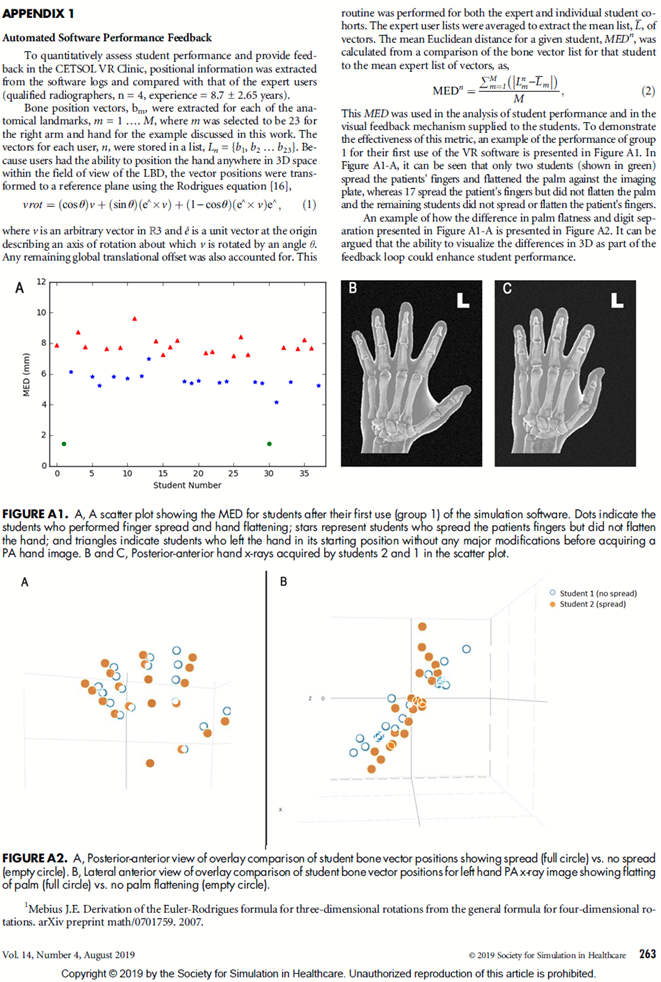
Introduction: Immersive virtual reality (VR) simulation environments facilitate novel ways for users to visualize anatomy and quantify performance relative to expert users. The ability of software to provide positional feedback before a practitioner progresses with subsequent stages of examinations has broad implications for primary and allied healthcare professionals, particularly with respect to health and safety (eg, exposing to x-rays). The effect of training student-radiographers (radiology technicians), with a VR simulation environment was quantitatively assessed.
Methods: Year 1 radiography students (N = 76) were randomly split into 2 cohorts, each of which were trained at performing the same tasks relating to optimal hand positioning for projection x-ray imaging; group 1 was trained using the CETSOL VR Clinic software, whereas group 2 was trained using conventional simulated role-play in a real clinical environment. All participants completed an examination 3 weeks after training. The examination required both posterior-anterior and oblique hand x-ray positioning tasks to be performed on a real patient model. The analysis of images from the examination enabled quantification of the students' performance. The results were contextualized through a comparison with 4 expert radiographers.
Results: Students in group 1 performed on average 36% (P < 0.001) better in relation to digit separation, 11%(P ≤ 0.001) better in terms of palmflatness and 23%(P ⩽ 0.05) better in terms of central ray positioning onto the third metacarpal. Conclusion: A significant difference in patient positioningwas evident between the groups; the VR clinic cohort demonstrated improved patient positioning outcomes. The observed improvement is attributed to the inherent task deconstruction and variety of visualization mechanisms available in immersive VR environments.
(Sim Healthcare 14:258–263, 2019)
A Comparison of User Perceptions VR SLE vs Traditional Clinical Role-Play Using Real World Laboratory Equipment
Virtual reality versus conventional clinical role-play for radiographic positioning training: A students' perception study
Sapkaroski, D., Mundy, M., & Dimmock, M. R. (2020). Virtual reality versus conventional clinical role-play for radiographic positioning training: A students' perception study. Radiography, 26(1), 57-62. doi:10.1016/j.radi.2019.08.001
Aim: The aims of this qualitative descriptive study were to 1) explore and define radiographers' competence in intravenous pharmacotherapy before and after a simulation-based education, 2) examine radiographer's perceptions of transfer of learning into clinical practice.
Method: Sixteen diagnostic radiographers in one hospitals' Clinical Radiology Unit were individually interviewed before a multidisciplinary simulation-based pharmacotherapy education intervention in 2012 and fourteen were re-interviewed after the intervention 6-7 months later. Data was analyzed using qualitative content analysis. Results: Before education the participants reported uncertain competence in pain management during imaging procedures and acute situations. These weak competence areas identified were strengthened and self-confidence grew. The intervention improved the domains of pharmacotherapy-related patient safety; teamwork development and communication skills. In addition, the radiographers indicated that the iv. pharmacotherapy knowledge from simulation learning was transferred to routine work.
Conclusion: The results of this study suggest simulation-based education is suitable for radiographers' pharmacotherapy learning. Adequate pain measurement and management are essential during invasive procedures and these skills can be realistically learned in simulations and transferred to clinical practice.
Translatable Clinical Outcomes
Immersive virtual reality simulated learning environment vs role play for empathic clinical communication training
Sapkaroski, D., Mundy, M., & Dimmock, M. R. (2020). Immersive virtual reality simulated learning environment vs role play for empathic clinical communication training (Currently under review)
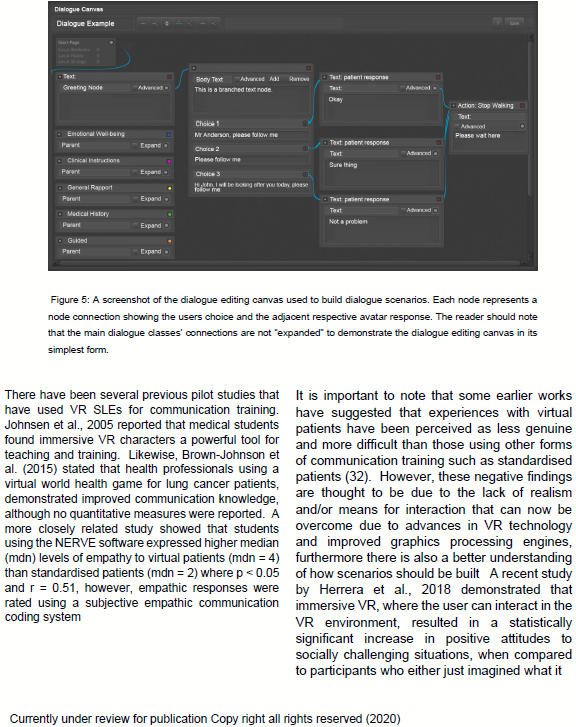
Introduction: The use of immersive virtual reality simulated learning environments (VR SLEs) for improving clinical communication can offer desirable qualities including repetition and determinism in a safe environment. The aim of this study was to establish whether the mode of delivery, VR SLE versus clinical role-play, could have a measurable effect on clinical empathic communication skills for a specific medical imaging scenario.
Methods: A randomised split-cohort study was performed with trainee practitioners (n=70) and qualified practitioners (n=9).
Results: Participants in the Trainee (TVR) and Clinician (CVR) groups using the VR intervention reported 11% and 12% improvements post training (p < 0.05), when compared to those assigned to the role-play intervention. Empirical assessment of communication training scores showed that participants in the TVR group performed 5% better on average than their role-play counterparts (p < 0.05).
Conclusion: The level of empathic language used by participants was shown to differ following a training intervention designed to improve interactions with patients that present for an MRI scan.
Practice implications
The ability to practice clinical communication scenarios in an individualised immersive VR experience without the judgment of peers, may lead to significant improvement in clinical communication skills over standardised role-play.